Dr. Rodrigo Bazúa Lobato

Introduction
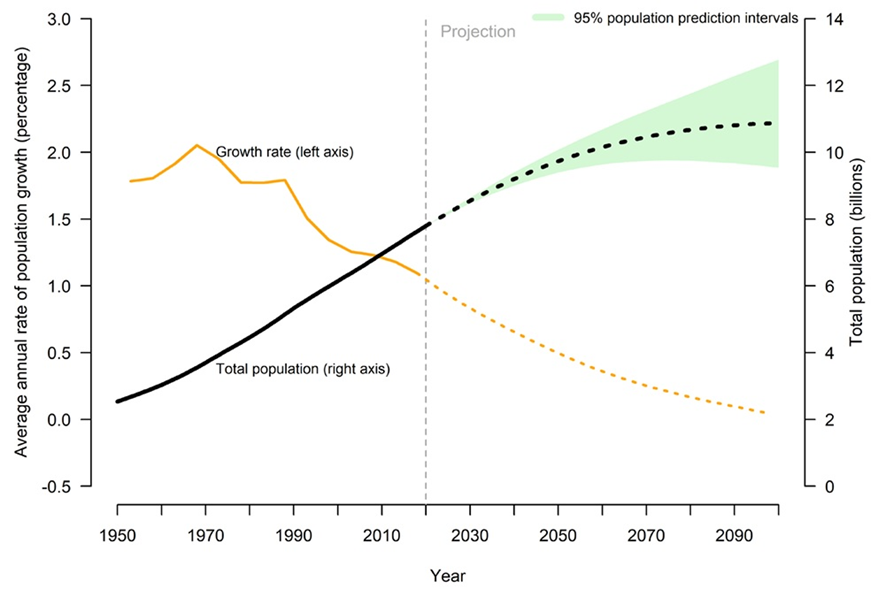
Health systems are at a global crossroads due to significant demographic, epidemiologic, climatic, and technological changes. On the demographic front, the world’s population has doubled over the past 50 years and is expected to double again by 2050 in some regions (World Bank, 2018). The globe has also experienced a continuous decrease in fertility rates and an increase in life expectancy, leading to an older global population (World Bank, 2022).
Epidemiologically, the leading causes of disease and mortality have dramatically changed. In 1990, 34% of global deaths were caused by communicable, maternal, neonatal, and nutritional diseases, which primarily affect children and pregnant women, while 56% were due to non-communicable diseases affecting mainly adults and older individuals. In contrast, by 2019, deaths from communicable, maternal, neonatal, and nutritional diseases had decreased to 18%, while deaths caused by non-communicable diseases had risen to 74% of total deaths (Global Burden of Disease Collaborative Network, 2020). Figure 1 illustrates the demographic transition.
Simultaneously, climate change is dramatically changing weather patterns and accelerating local and international migration by generating extreme weather events, including floods, heat waves, droughts, wildfires, and intensifying water stress (Prange, 2022), which by 2050 could force 216 million people to migrate within their countries (World Bank, 2021) To put it in perspective, of the 46.9 million people internally displaced in 2023, 56% were driven to migrate due to natural disasters linked to climate change (Internal Displacement Monitoring Centre, 2024).
Furthermore, a dramatically accelerating technological change, particularly related to digital technologies, including increasing internet accessibility, social media penetration, robotics, and artificial intelligence capabilities, is quickly changing how we live and interact with each other and our environments. This technological revolution is both generating new health challenges and creating new possibilities to address major health needs (Valkenburg, Meier, & Beyens, 2022; Alowais et al., 2023).
Along with the major demographic, epidemiologic, climatic, and technological changes mentioned above, over the last centuries, the world has experienced a major shift in how societies respond to the health needs of individuals through policies and institutions, which, for most of history, had been limited to the household and carried out by the family nucleus. In 1883, Bismarck instituted the first social security health insurance scheme for guild workers in Germany, framing healthcare as a right for workers to keep them healthy and productive, and as an instrument to prevent strikes. In 1948, Beveridge established the National Health Service in Britain, representing the first health institution covering the whole population of a country through general taxation, focused on solidarity, social cohesion, and universality (Delnoij, 2013).
In addition to country-specific organized social responses to the health needs of the collectivity, the world saw the birth of a new way of conceptualizing and institutionalizing the inherent value of human life and the human right to health, first articulated in the 1946 Constitution of the World Health Organization (WHO), and reaffirmed in 1948 with the Universal Declaration of Human Rights, adopted in the aftermath of the Second World War (World Health Organization, 1946; United Nations, 1949).
The aspiration of the human right to “the enjoyment of the highest attainable standard of physical and mental health […] without distinction of race, religion, political belief, economic or social condition” (World Health Organization, 1946) is still far from being realized. To continue the progress towards attaining the right to health for all in a rapidly changing global landscape requires creating policies and institutions that operationalize the inherent value of every life.
The remainder of this article first provides an overview of the unequal global distribution of the burden of disease and the resources to address it. It is followed by a review of the long struggle for health equity. The third section briefly presents the progress made towards achieving the right to health for all. The article ends with an exploration of how the long walk to achieving the right to healthhealth could be continued by expanding the ideals of humanism with neohumanism.
The Unequal Distribution of the Global Burden of Disease and of the Resources to Address It
The global distribution of disease follows patterns of geographic and social clustering of morbidity and mortality related to ecologic, economic, social, and political factors, among others. The life expectancy of a child born in 2021 in Japan, Liechtenstein, Switzerland, and South Korea was 84 years, while a child born in Chad, Nigeria, and Lesotho had a life expectancy of 53 years (World Bank, 2021). These disparities are also observed within countries and smaller geographical units. For example, at the local level, in the city of Boston, in the United States, life expectancy in the affluent neighborhood of Back Bay is nearly 92 years, while it decreases by 23 years in the poorer neighborhood of Roxbury, with a life expectancy of 69 years (Boston Public Health Commission, 2023).
This disparity in life expectancy is primarily driven by a higher burden of disease in poorer countries and localities, coupled with limited resources to address it. The overall burden of disease worldwide is highest in low- and middle-income countries (LMICs), which have the least resources for healthcare. While 77% of global deaths due to non-communicable diseases occur in low- and middle-income countries (World Health Organization, 2022), LMICs spent in 2019 between $34 and $551 USD per capita on healthcare, a minimal amount compared to the $5,635 USD spent per capita on healthcare in high-income countries in that same year (World Bank, 2022). Figure 2 shows the total burden of disease by country in 2019, measured in total disability-adjusted life years (DALYs) from all causes per 100,000 individuals. One DALY represents the loss of the equivalent of one year of full health, either due to years of life lost due to premature mortality (YLLs) and years of healthy life lost due to disability (YLDs) due to prevalent cases of the disease or health condition in a population (WHO, n.d.).

Although it is outside the scope of this article to explore the historical forces that have shaped the aforementioned global inequalities, it will be only mentioned here that the inequalities observed have been significantly shaped by slavery, colonialism, resource extraction, and other different forms of oppression, which selectively benefitted a few and profoundly disenfranchised large part of the global population, among other factors (Mukherjee, 2021).
The Long Path to Health as a Human Right
As was mentioned in the introduction, for most of history, responding to the health needs of individuals in a community or a society had not been a collectively organized endeavor but rather limited to the household and carried out by the family nucleus. The first recorded collective responses to disease were focused on prevention efforts related to the provision of clean water, sanitation, and the management of “pestilential” diseases, such as the Roman aqueducts and the implementation of “quarantines” or isolation of individuals suffering from what would be considered infectious diseases nowadays (Porter, 2005). However, some of the first documented organized collective responses to treating disease for “others” can be found during the expansion of European empires and colonialism, as health was a priority of European imperial endeavors in the New World, Africa, and Asia (Rose, 2001).
Colonial medicine was first developed to support colonial military endeavors and then expanded to protect the health of the laboring populations required for large plantations and mines to operate. For example, Britain established a Colonial Medical Service, with clinics in particular areas of the empire, recruiting physicians trained in England to work in the colonies. The facilities offered curative medicine, public health campaigns, and collected data regarding epidemics (Crozier, 2007). European colonial health efforts were both directed at treating disease and at “implanting” disease. For instance, British officials were documented distributing blankets intentionally infected with smallpox to American indigenous people as late as 1763 (Jones, 2004).
Alongside the expansion of colonial empires worldwide, effective drugs for previously incurable diseases and microorganisms as causative disease agents were discovered, extending medicine’s capabilities, such as the advent of quinine as an effective treatment for malaria, which allowed European colonialists to expand their colonization of the tropics further. With these developments, by the end of the 19th century, western medicine had been split into “tropical medicine,” which focused on specific diseases found in tropical latitudes, many transmitted by vectors, and “cosmopolitan medicine,” which addressed diseases that mostly occurred in Europe or anywhere in the world, like tuberculosis (Worboys, 1976).
Colonial, tropical, and cosmopolitan medicine were not the only healthcare models during the colonial period. Missionary medicine, in contrast to colonial medicine’s economic incentive, was primarily provided on moral grounds. Missionaries focused on Western culture, hygiene, early biomedicine, and Christianity as a solution to illness and a pathway to salvation (Farmer et al., 2013).
During the 18th and 19th centuries, with the beginning of the fragmentation of European empires, the independence of previous colonies, and the rise of the United States as a global power, came a significant increase in international maritime trade. These developments incentivized collaboration between countries to exchange epidemiological information. In the Americas, the main concerns were the arrival of yellow fever, cholera, and the bubonic plague through ports. As a result, the first international organization focused on health and inter-country collaboration for preventing disease was born in 1902, the Pan American Sanitary Bureau, which later became the Pan American Health Organization (Cueto, 2006).
At the international level, only in the aftermath of the Second World War did collective efforts to protect human health globally shift from primarily economic concerns, such as allowing safe international trade by controlling the spread of infectious diseases through epidemiologic intelligence. In 1948, the Universal Declaration of Human Rights (UDHR) was adopted as an aspirational but not legally binding document to prevent the events of the Second World War from occurring again. It underlined that all human rights are interdependent and that they cannot be hierarchically ordered.
One year later, legally binding documents on human rights were drafted for all United Nations member states to adopt formally. Still, the two predominant world powers, the United States and the Soviet Union, could not agree on a single document. While the United States favored rights such as freedom of expression and association, the Soviet Union claimed that the right to education and health were more important than those favored by the United States.
Consequently, the formalization of legally binding documents on human rights was postponed until 1966, when two legally binding treaties on human rights were signed. These treaties divided the UDHR into two covenants: the International Covenant on Civil and Political Rights (ICCPR) and the International Covenant on Economic, Social, and Cultural Rights (ICESCR), the first one endorsed by the United States and the second one endorsed by the Soviet Union. The Soviet Union signed and ratified the ICCPR years later (United Nations, 1966), while the United States has not ratified the ICESCR to this day (Piccard, 2010).
The countries aligned with or under the influence of the United States signed the ICCPR, and those aligned with or under the influence of the Soviet Union signed the ICESCR. The human right to health was only found in the ICESCR in its article 12, which defines it as the enjoyment of the highest attainable standard of physical and mental health (ICESCR, 1966).
“Planetary Health is one of the first attempts at expanding the underlying spirit of humanism to other animate and inanimate entities at the global academic and policy levels.”
The Right to Health: From Paper to Practice
In 1978, the World Health Organization organized an international conference on Primary Health Care in Alma-Ata, Kazakhstan, to strengthen the idea that every human being deserves health access, backed primarily by the Soviet Union. The conference produced the Declaration of Alta-Ata, which stated the commitment of the 134 signing countries, including the United States and the Soviet Union, to bring primary health care to everyone under the slogan “health for all by the year 2000” (Farmer et al., 2013).
The Declaration included in the definition of Primary Health Care the following elements: “education concerning prevailing health problems and the methods of preventing and controlling them; promotion of food supply and proper nutrition; an adequate supply of safe water and basic sanitation; maternal and child health care, including family planning; immunization against the major infectious diseases; prevention and control of locally endemic diseases; appropriate treatment of common diseases and injuries; and provision of essential drugs” (World Health Organization, 1978a).
Even though several countries made progress in expanding access to health care, the progress expected by 2000 was not achieved. One major factor for the nonsuccess of the Declaration was that it did not specify the financial mechanisms to pay for primary health care and its scale-up worldwide. Only one paragraph of its 80 pages discussed financing as follows: “The affluent countries would do well to substantially increase the transfer of funds to the developing countries for primary health care” (World Health Organization, 1978b).
Another factor hindering the success of the Declaration of Alma-Ata was a parallel effort led by the Rockefeller Foundation. The Rockefeller Foundation organized a global Conference in Bellagio, Italy, months after the Alma-Ata Conference, to discuss the impact of population growth on health. However, the product of this conference was an alternative plan to improve health worldwide, which contrasted with the goal of “primary health care for all by the year 2000.” The Bellagio conference championed the concept of Selective Primary Care, which offered an alternative to the comprehensive view of Primary Health Care offered by the Declaration of Alma-Ata. This alternative view focused more on the notion of “cost-effectiveness” rather than on the overall needs of people, identifying a package of discrete services that would offer high returns in lives saved per dollar spent (Farmer et al., 2013).
A third factor halting the progress toward health for all was the rise of economic neoliberalism worldwide during the 1980s, coupled with an international debt crisis. Developing countries across the globe were incentivized to conduct “structural adjustment” policies by the World Bank and the International Monetary Fund (IMF), which dramatically increased the amount and magnitude of loans they provided to developing countries, with the condition of adhering to specific economic policies and government structures, which emphasized market-oriented policy reforms and a diminished role for the state as a provider of services, such as healthcare (Farmer et al., 2013).
With these reforms, health care was defined as a commodity, not a right, which should be allocated by the market, favoring Selective Primary Care for the impoverished and underserved. The impact of the structural adjustment policies on healthcare was most severely suffered by the poor in developing countries. For instance, researcher David Struckler, King & Basu (2008) estimated that participating in a structural adjustment program was associated with an 8% decrease in government spending as a percentage of gross domestic product, a 7% drop in the number of physicians per capita, and a 42% drop in the percentage of the population covered by directly observed therapy for tuberculosis control (Struckler, King & Basu, 2008).
A new momentum for the right to health came with the turn of the century when, in September 2000, the United Nations presented the Millennium Development Goals (MDGs). The MDGs were a list of eight goals for member states and development partners to achieve by 2015. Four of these goals were partially or directly related to health: the eradication of extreme poverty and hunger, reduction of child mortality, improvement of maternal health, and combating HIV/AIDS, malaria, and other diseases. MDGs brought an unprecedented mobilization of resources globally, fueling a 66% increase in official development assistance between 2000 and 2014. The goals also informed global health priorities and incentivized the formation in 2002 of the Global Fund to Fight Aids, Tuberculosis and Malaria. With the MDGs, from 1990 to 2015, the prevalence of undernourishment in children went from 23% to 13%, child mortality fell by 53% and maternal mortality by 43%, and the targets for HIV, TB, and malaria were met (World Health Organization, 2015).
Even though the MDGs generated significant momentum towards improved health for all, they fell short of recognizing that progress towards the right to health must be broader than focusing on a limited set of health needs and conditions. With this in mind, with the arrival of the MDGs target time (2015), the United Nations adopted a revised development agenda, which included 17 Sustainable Development Goals (SDGs) to be achieved by 2030 (World Health Organization, 2015).
In the SDGs, there was only one health goal (goal number three), which was deliberately framed with a much broader approach than the health goals of the MDGs: Ensure healthy lives and promote well-being for all at all ages. This SDG also included specific targets, one of which is Universal Health Coverage (UHC), exemplifying the need to extend health care for all from basic, cost-effective interventions to consider the broad spectrum of health needs that generate a substantial amount of the burden of disease (World Health Organization, 2015).
Universal health coverage seeks to ensure that every person has access to the quality health services they need, when and where they need them, including during emergencies, without risk of financial hardship. Furthermore, according to the WHO, UHC involves the entire continuum of care, including health promotion, prevention, treatment, rehabilitation, and palliative care (World Health Organization, 2023).
Even though UHC is a much more comprehensive aspiration to address human health needs, progress towards achieving it has been limited, particularly since 2015. According to the WHO, improvements to health services coverage have stagnated since 2015, the proportion of the population that faced catastrophic health expenditures has increased since 2000 across all regions and the majority of countries. Additionally, the proportion of the population not covered by essential health services decreased by about 15% between 2000 and 2021, with negligible improvements made after 2015, leaving about 4.5 billion people, the majority of the world’s population, without access to essential health services (World Health Organization, 2023).
Neohumanism as a Framework Forward to Achieve the Right to Health
As has been covered in this article, the last centuries have experienced a steady progression towards creating policies, institutions, and systems that increasingly recognize the right of every human being to health and the need to protect it. However, it has also been covered that the objective of bringing health care for all is far from being achieved, with the majority of human beings still not having access to essential health services.

One way to explain the mismatch between the global recognition of the human right to health and the lack of actually achieving it for all is that this mismatch is a reflection of how the globalization process has taken place under an international system of dependency.
Dependency in global affairs refers to “a situation in which the economy of certain countries is conditioned by the development and expansion of another economy to which the former is subjected. The relation of inter-dependency between two or more economies, and between these and world trade, assumes the form of dependency when some countries (the dominant ones) can expand and can be self-sustaining, while other countries (the dependent ones) can do this only as a reflection of that expansion, which can have either a positive or a negative effect on their immediate development” (Dos Santos, 1970).
Considering as a starting point the year 1950, two years after the adoption of the UDHR, when the per capita income of the industrialized, developed, or dominant countries was $3,841 USD, while that of the low-income, developing or dependent countries was $146 USD, we may observe that the trajectories of dominant and dependent countries were starkly different. Although thirty years later, in 1980, the per capita income in dominant countries had expanded to $9,648, the per capita income in dependent countries only rose to $245. In thirty years, the gap in per capita income gap between dominant and dependent countries grew from $3,695 to $9,403 USD (Namkoong, 1999).
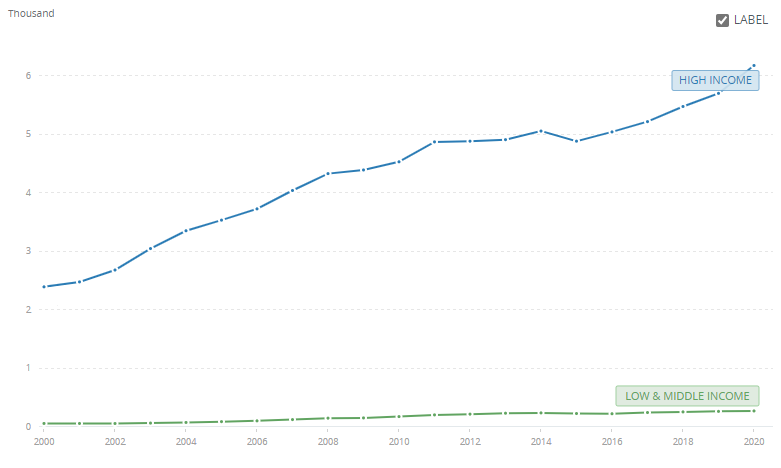
Following this comparison, we find a similar progression when we observe the dynamics of health expenditure per capita. While in the year 2000, the per capita health expenditure in low and middle-income countries (dependent) was $60.57 USD, the same measure was $2,394.95 in high-income countries (dominant). By the year 2020, this figure had increased to $274.28 in dependent countries and to $6,176.46 in dominant countries, expanding the gap from $2,334.38 to $5,902.18 USD (World Bank, 2024). Figure 3 shows the per capita health spending trajectories in dominant and dependent countries.
As Figure 2 depicts, similar patterns in the distribution of the burden of disease can be observed between dominant and dependent countries, where dominant countries are healthier and dependent countries are sicker.
The neohumanist philosophy of P.R. Sarkar describes two main sentiments that underlie the significant gap between countries and between socioeconomic and ethnic groups in terms of wealth and health. Sarkar refers to the socio-sentiment and the geo-sentiment as the identification with and having higher esteem with a particular sociological group and geographical place, respectively (De Oliveira, 2023).
These sentiments underlie why, even though there has been a global recognition of the fundamental right to health of every human being for 76 years, the unprecedented economic expansion that the world has experienced over the last century has not translated into an equal expansion of health services available to the impoverished and underserved of the world, as wealth and disease follow social and geographical patterns.
If we want to progress forward to achieve the right to health for all, under the current trends of migration, climatic change, and technological transformations, it will be imperative for the global health policy framework to evolve in its institutional structures. One major flaw of the existing global policy framework related to the right to health is that they are primarily limited to setting aspirations and goals, without clear channels of global cooperation to materialize them. The next global institutional requirement to achieve the right to health is to generate a global health institutional network that operates not only at goal setting, but also at other levels of traditional health systems structures, including mechanisms for global financing, payment, organization of healthcare delivery, and regulations, guided by a clear neohumanist ideal that excludes any geo- and socio-sentiments, but rather exalts the equal value and dignity of each human live.
Lastly, P.R. Sarkar’s neohumanist philosophy extends beyond humanism, beyond recognizing the inherent value of each human life, but also recognizes the inherent value of each living being on this earth, and even the inherent value of the non-living matter. In his seminal work on neohumanism, Sarkar states:
…when the underlying spirit of humanism is extended to everything, animate and inanimate, in this universe – I have designated this as “Neohumanism.” This Neohumanism will elevate humanism to universalism, the cult of love for all created beings of this universe.
(Sarkar, 1982)
The movement towards this universal aspiration has already started in the academic health sciences sphere, under the terms “Planetary Health” and “One Health,” championed by different institutions (de Castañeda et al., 2023). One Health historically focused on zoonoses, proposed and led by veterinary communities, however, the concept has continuously developed. One Health is currently defined by the Food and Agriculture Organization, the UN Environment Programme, and WHO as “an integrated, unifying approach that aims to sustainably balance and optimize the health of people, animals, and ecosystems. It recognizes the health of humans, domestic and wild animals, plants, and the wider environment (including ecosystems) are closely linked and interdependent. The approach mobilizes multiple sectors, disciplines, and communities at varying levels of society to work together to foster well-being and tackle threats to health and ecosystems, while addressing the collective need for healthy food, water, energy, and air, taking action on climate change and contributing to sustainable development” (One Health High-Level Expert Panel et al. 2022).
Planetary Health has been championed by the Rockefeller Foundation and the medical journal The Lancet. It recognizes that the impact of human activities on our planet’s natural systems has led to the disruption and transformation of most natural systems, including the disruption of the global climate system; widespread pollution of air, water, and soils; rapid biodiversity loss; reconfiguration of biogeochemical cycles, including that of carbon, nitrogen, and phosphorus; ecosystems destruction and transformation; changes in land use and land cover, and resource scarcity, including that of fresh water and arable land (Myers, 2017). These disruptions are not only leading to the sixth major extinction of living species since the formation of our planet, but they also represent a serious threat to human health (Pievani, 2014). Planetary health recognizes that human health and well-being depend on protecting and restoring the natural environment we inhabit and share with other species on this planet.
While Planetary Health and One Health still revolve around human health, they represent some of the first attempts at expanding the underlying spirit of humanism to other animate and inanimate entities at the global academic and policy spheres. The struggle for the recognition of the human right to health was a multi-century effort that was catalyzed by the abominable events of the Second World War. It was not only an intellectual development, but rather it required a new ethical and philosophical conception of humanity under humanism, enshrined in the universal declaration of human rights.
We are living at times of abominable destruction of human lives, non-human lives and inanimate members of our planet. Global efforts recognizing the need to protect all lives as a shared international priority are quickly developing and expanding, but have lacked a comprehensive guiding philosophical and ethical viewpoint that could bring them to the general public. The time is ripe for a new ethical and philosophical viewpoint for all of humanity to reassess its relationship with the rest of the world, one which expands the spirit of humanism to everything, animate and inanimate, such as nehumanism.
After all, as Dr. Paul Farmer stated, “The idea that some lives matter less is the root of all that is wrong with the world.”
References
Alowais, S. A., Alghamdi, S. S., Alsuhebany, N., Alqahtani, T., Alshaya, A. I., Almohareb, S. N., Aldairem, A., Alrashed, M., Bin Saleh, K., Badreldin, H. A., Al Yami, M. S., Al Harbi, S., & Albekairy, A. M. (2023). Revolutionizing healthcare: the role of artificial intelligence in clinical practice. BMC medical education, 23(1), 689. https://doi.org/10.1186/s12909-023-04698-z
Boston Public Health Commission (2023). Health of Boston 2023. https://www.boston.gov/sites/default/files/file/2023/05/HOB_Mortality_LE_2023_FINAL_May12.pdf
De Oliveira, M.A. (2023). What’s Neo About Neohumanism?. Neohumanist Review. https://theneohumanist.com/2023/06/24/160/
Crozier, A. (2007). Practising colonial medicine: The colonial medical service in British East Africa. Bloomsbury Publishing.
Cueto, M. (2006). The value of health: a history of the Pan American Health Organization. PAHO.
de Castañeda, R. R., Villers, J., Guzmán, C. A. F., Eslanloo, T., de Paula, N., Machalaba, C., Zinsstag, J., Utzinger, J., Flahault, A., & Bolon, I. (2023). One Health and planetary health research: leveraging differences to grow together. The Lancet. Planetary health, 7(2), e109–e111. https://doi.org/10.1016/S2542-5196(23)00002-5
Delnoij D. M. (2013). Bismarck or Beveridge: primary care matters. European journal of public health, 23(3), 349. https://doi.org/10.1093/eurpub/ckt021
Dos Santos, T. (1970). The structure of dependence. American economic review, 60(2), 231.
Farmer, P., Kim, J. Y., Kleinman, A., & Basilico, M. (2013). Reimagining global health: an introduction (Vol. 26). Univ of California Press.
Global Burden of Disease Collaborative Network. (2020). Global Burden of Disease Study 2019 Results.
Institute for Health Metrics and Evaluation.https://vizhub.healthdata.org/gbd-results/
Internal Displacement Monitoring Centre (2024). Global Report on Internal Displacement. Internal Displacement Monitoring Centre.https://www.internal-displacement.org/global-report/
Jones, D. S. (2004). Rationalizing epidemics: meanings and uses of American Indian mortality since 1600. Harvard University Press.
Mukherjee, J. (2021). An introduction to global health delivery: practice, equity, human rights. Oxford University Press.
Myers S. S. (2017). Planetary health: protecting human health on a rapidly changing planet. Lancet (London, England), 390(10114), 2860–2868. https://doi.org/10.1016/S0140-6736(17)32846-5
Namkoong, Y. (1999). Dependency theory: Concepts, classifications, and criticisms. International Area Review, 2(1), 121-150.
One Health High-Level Expert Panel (OHHLEP), Adisasmito, W. B., Almuhairi, S., Behravesh, C. B., Bilivogui, P., Bukachi, S. A., Casas, N., Cediel Becerra, N., Charron, D. F., Chaudhary, A., Ciacci Zanella, J. R., Cunningham, A. A., Dar, O., Debnath, N., Dungu, B., Farag, E., Gao, G. F., Hayman, D. T. S., Khaitsa, M., Koopmans, M. P. G., … Zhou, L. (2022). One Health: A new definition for a sustainable and healthy future. PLoS pathogens, 18(6), e1010537. https://doi.org/10.1371/journal.ppat.1010537
Pievani, T. (2014). The sixth mass extinction: Anthropocene and the human impact on biodiversity. Rendiconti Lincei, 25, 85-93.
Piccard, A. M. (2010). The United States’ Failure to Ratify the International Covenant on Economic, Social and Cultural Rights: Must the Poor Be Always with Us?. Scholar, 13, 231.
Porter, D. (2005). Health, civilization and the state: a history of public health from ancient to modern times. Routledge.
Prange, M. (2022). Climate Change Is Fueling Migration. Do Climate Migrants Have Legal Protections? Council on Foreign Relations. https://www.cfr.org/in-brief/climate-change-fueling-migration-do-climate-migrants-have-legal-protections
Rose, N. (2001). The politics of life itself. Theory, culture & society, 18(6), 1-30.
Sarkar, P. R. (1982). The liberation of intellect: Neo-humanism. Ananda Marga Pracaraka Samgha.
Stuckler, D., King, L. P., & Basu, S. (2008). International Monetary Fund programs and tuberculosis outcomes in post-communist countries. PLoS medicine, 5(7), e143.
United Nations. General Assembly. (1949). Universal declaration of human rights.
United Nations (1966). International Covenant on Civil and Political Rights. United Nations
Treaty Collection. https://treaties.un.org/Pages/showDetails.aspx?objid=0800000280004bf5
Valkenburg, P. M., Meier, A., & Beyens, I. (2022). Social media use and its impact on adolescent mental health: An umbrella review of the evidence. Current opinion in psychology, 44, 58–68. https://doi.org/10.1016/j.copsyc.2021.08.017
Worboys, M. (1976). The emergence of tropical medicine: a study in the establishment of a scientific specialty. Perspectives on the emergence of scientific disciplines, 75-98.
World Bank. (2018). A changing world population. World Bank
World Bank. (2021). Climate Change Could Force 216 Million People to Migrate Within Their Own Countries by 2050
World Bank. (2022). Societal Aging. World Bank
World Bank (2024). Current health expenditure per capita (current US$) – High income, Low & middle income. World Bank
World Health Organization. (1946). The constitution of the world health organization.
World Health Organization. (1978a). Declaration of alma-ata (No. WHO/EURO: 1978-3938-43697-61471). World Health Organization. Regional Office for Europe.
World Health Organization. (1978b). Primary health care: report of the International Conference on primary health care, Alma-Ata, USSR, 6-12 September 1978. World Health Organization.
World Health Organization. (2022). Noncommunicable diseases. World Health Organization
World Health Organization (2015). From MDGs to SDGs: General Introduction. World Health Organization
World Health Organization (2023). Universal Health Coverage. World Health Organization
World Health Organization (n.d.). Global health estimates: Leading causes of DALY. Global Health Observatory
Rodrigo Bazúa Lobato is a Mexican primary-care physician and public health professional committed to social justice and the right to high-quality healthcare for all, working with the Mexican Government in its ongoing Healthcare Reform. He has worked in remote rural clinics in Southern Mexico as a clinician and developing community health programs. Additionally, Rodrigo worked with the United Nations High Commissioner for Refugees during the COVID-19 pandemic as a medical advisor. He was awarded the Gustavo Baz Award to Social Service in 2016 by the National Autonomous University of Mexico, and the Excellence in Health and Nutrition Scholarship 2011-2016 by the “Carlos Slim” Institute of Health. He was a New Voices Fellow 2018 with the Aspen Institute and a Global Health Fellow 2017-2019 with the HEAL Initiative.

